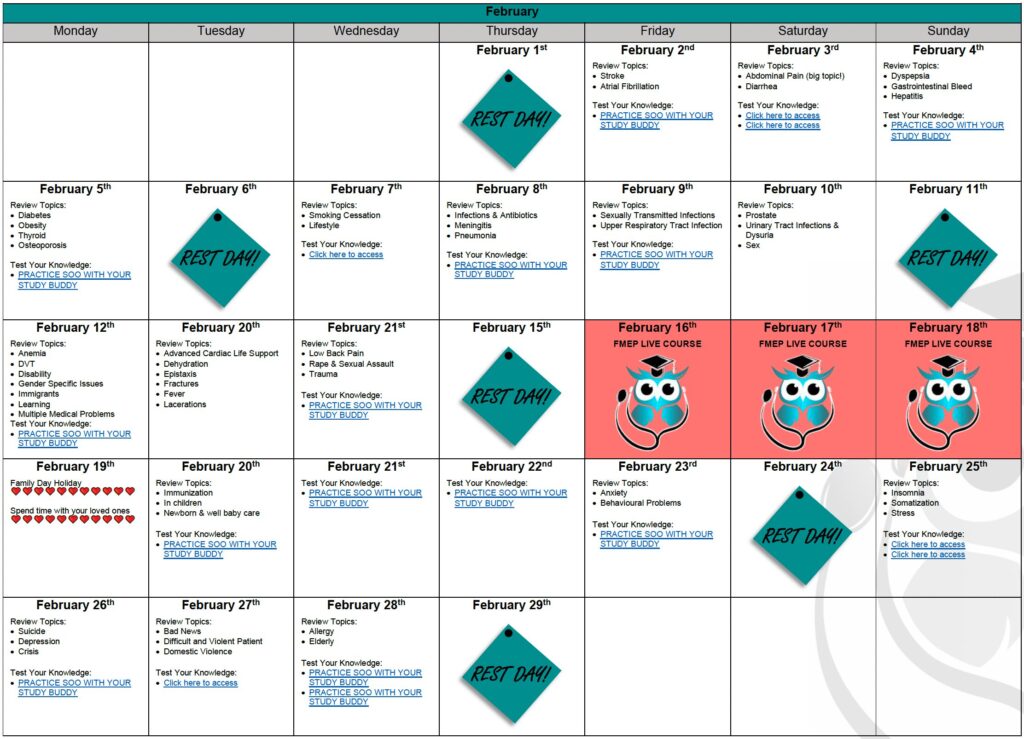
YOUR DETAILED CCFP EXAM STUDY CALENDAR: BE PREPARED!
The CCFP exam is quickly approaching. We know you are juggling many personal and professional...
Comments Off on YOUR DETAILED CCFP EXAM STUDY CALENDAR: BE PREPARED!
Just a reminder… pay attention to the questions. Here are our general tips one more time:
1. Pay attention to the questions. Look carefully at how many items you are being asked to list. If the question asks for five items, you will not get more marks if you list eight items; the examiner will look at the first five and allocate marks only for the first five answers – so be careful. On a SAMP, if it is not clearly stated how many items you should list, look at the amount of points/marks being allocated for the question to get an idea of how many answers the examiner may be anticipating you write down.
2. Do not write lengthy answers. Most questions can be answered in 10 words or less!
3. Be specific when writing down investigations (hemoglobin instead of CBC; CT abdomen instead of CT).
4. Remember that trade names and generic names are both acceptable when writing down medications.
5. For more helpful tips, you can refer to CCFP’s SAMP instructions by clicking here.
SAMP
Janet is a 32 year old G1P1, who delivered her newborn baby 4 weeks ago. The baby has had excellent weight gain since birth and she has been exclusively breastfeeding. She is here for the 1-month follow-up and has a number of questions. (10 points)
1. She went to the pharmacy but forgot the amount of vitamin D she should give to her baby. For infants who are exclusively breastfed, what is the recommended vitamin d supplementation? (1 point)
2. At times, the baby has difficulty with the latch. What are two ways to optimize the latch and improve success with breastfeeding? (2 points)
3. She reports a tender nodule in her breast with some erythema. You examine her and her right breast has mild erythema and is tender to palpate. She is otherwise well. How would you manage? (1 point)
4. She reports plaques on the baby’s tongue. You try to remove them with a tongue depressor but are unable to do so. How would you manage? (1 point)
5. What are three contraindications to breastfeeding? (3 points)
6. She asks about her contraceptive options while breastfeeding. What two options could you offer? (2 points)
Helpful Resources:
1) Breastfeeding Challenges and Newborn Nutrition, Feb 2021, Practice Based Small Group Learning Program. www.fmpe.org.
2) https://www.jogc.com/article/S1701-2163(16)39786-9/pdf
3) https://cdn.dal.ca/content/dam/dalhousie/pdf/faculty/medicine/departments/core-units/cpd/academic-detailing/ADS_2015_Contraception_Workbook.pdf
4) https://www.gacguidelines.ca/site/GAC_Guidelines/assets/pdf/CONT05_-_Contraception_Summary_Mar_12_08.pdf