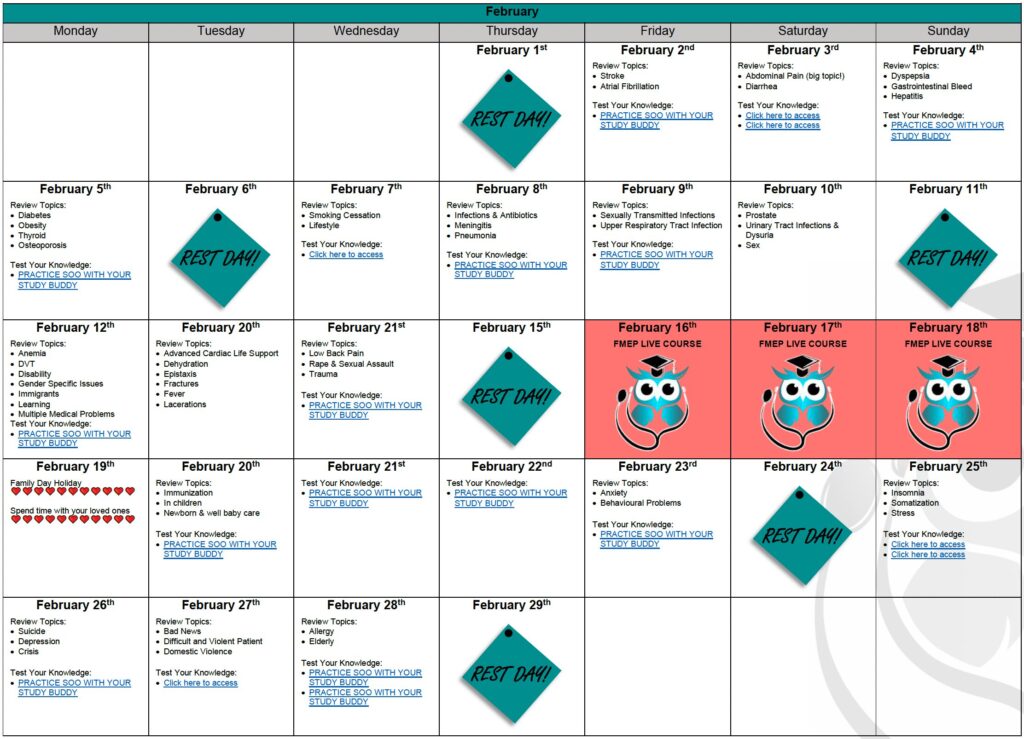
YOUR DETAILED CCFP EXAM STUDY CALENDAR: BE PREPARED!
The CCFP exam is quickly approaching. We know you are juggling many personal and professional...
Comments Off on YOUR DETAILED CCFP EXAM STUDY CALENDAR: BE PREPARED!
It’s the CCFP SOO exam – you’re about to enter the next station … Your station has a 23-year-old male coming in for travel advice. He is going to Jamaica and wants to know what he can do to prevent getting traveller’s diarrhea. What are you going to ask? Are you confident about what medications he needs? What investigations may be needed once the patient has returned home if the symptoms persist?
If you’re ready to learn how to become a FMEP course SUPERIOR Certificant… keep reading.Â
This blog is a summary of the Canadian Family Physicians’ article on traveller’s diarrhea. The article can be found here.
“Doc, what is traveller’s diarrhea?â€
Traveller’s diarrhea (TD), the quick onset of loose or liquid stools during travel, is a prevalent problem that can impact your travel plans. TD occurs when travellers consume food or beverages that are contaminated, typically by a bacteria pathogen (e.g., enterotoxigenic Escherichia coli, enteroaggregative E. Coli, or Campylobacter).
“Doc, what symptoms should I watch out for?â€
Symptoms can include cramps, stomach pain, urgent stools, fever, vomiting, and dysentery (bloody diarrhea). They tend to last 2-4 days.
“What steps can I take to reduce my risk?â€
You can advise the following:
Tell the patient to pack the following:
“Okay Doc, I will pack what you suggested. When do I take these medications?â€
“What happens if my symptoms persist despite your recommended treatments?â€
Written by Maria Veinberg. Reviewed by Dr. Prokubovskaya & Dr. Premji.