Before entering the next SOO station, you read the prompt: “You are about to meet a patient whose clinical presentation and investigations are suggestive of a new diagnosis of lupus.†You eloquently perform a review of systems, provide an excellent management plan and arrange follow up with the patient… But you are NOT deemed a SUPERIOR CERTIFICANT. What went wrong?It was actually a “Bad News†scenario, and you didn’t use interviewing techniques that the FMEP Course hopes to see in a SUPERIOR certificant.
The good news is that we have the tips and tricks you can use when a similar situation shows up on your exam. We have summarized an excellent AFP article that will help you be an FMEP Superior Certificant on your SOO.
How might “bad news†show up on your CCFP exam SOO station?
- You might need to need to disclose a new diagnosis of cancer
- You might need to inform them of a new diagnosis of a chronic disease (e.g., diabetes, hypertension, kidney failure)
- You may need to discuss the aftermath of an injury leading to significant life changes
- You may need to address a deteriorating condition and advise them that improvement is unlikely (e.g., end-stage chronic obstructive pulmonary disease, congestive heart failure, etc.)
- You might need to inform a family member that their loved one is unwell and may not recover
Some general tips for your SOO:
Before you memorize any mnemonics, remember these universal tips:
- Deliver the news in person (no kidding!)
- Use clear, easily comprehensible language
- Avoid medical jargon, like “Hodgkin lymphoma with metastatic spread.†This is not the right time to demonstrate that you know your oncological lymphoma staging. Check their understanding first by saying, “What have you been told so far about today’s encounter?â€
- Give the patient your full attention
- Do not write notes on your scratch pad while thinking about how to FIFE them. Look them in the eye. This should feel natural.
- Leave enough time for questions
- Involve the patient in their management plan
- Ensure that the patient feels heard
- Say things on your SOO like, “How does that sound?â€, “Do you have any questions?â€, and “Is there anything else you would want to add/address?â€
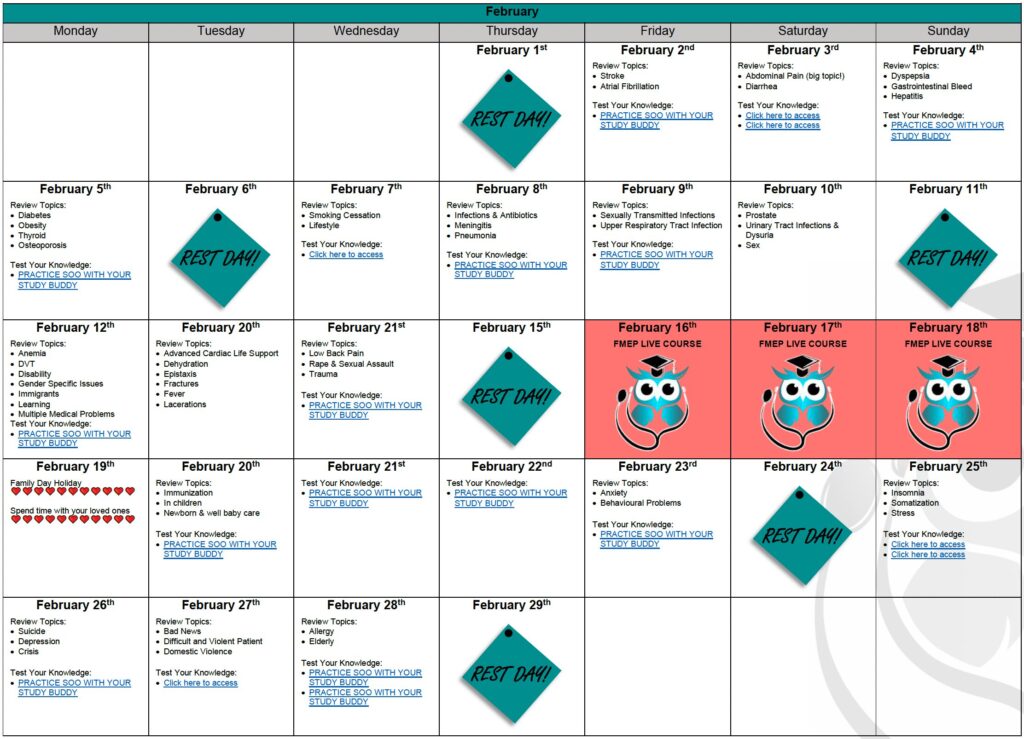
- We’ll give you more management tips and demonstrations of delivering bad news during the FMEP Course
- Be honest and realistic while remaining compassionate
How should I approach the “Bad News†SOO scenario?
Here’s where you might want to get memorizing! Let’s talk about SPIKES.
- Setting
- Review the patient’s medical history
- Use the tissues that will likely be close by
- Maintain eye contact
- Ask if the patient wants any loved one(s) present with them during the conversation
- Position yourself appropriately… “Would it be okay if I sat next to you?â€
- Perception
- Gauge how much the patient already knows about his/her condition and investigations to date
- Start with broad questions
- Consider… “What is your understanding of what I’ve told you about your MRI results?â€
- Invitation
- Ask if the patient is ready to hear the news (if not, arrange another appointment)
- Ask how much information the patient would like to hear
- Consider… “Do you have a preference on how much information you would like me to discuss with you today?â€
- Knowledge
- Use clear, simple language
- Be empathetic and allow the patient to express their emotions
- Provide small pieces of information, check in often to make sure the patient understands, and give the patient opportunities to ask questions
- Include a warning statement before delivering the news
- Consider… “Unfortunately, the test results are not what we were hoping to see.â€
- Emotions
- Acknowledge and accept the patient’s emotions
- Your response should be empathetic, validating, supportive, or exploratory, depending on their concerns
- Consider… “You mentioned you were worried about your husband. Could you tell me more about where this worry is coming from?â€
- Strategy and Summary
- Give a summary, discuss options, and explore patient-specific goals
- Arrange for follow-up (tests, referrals, treatments)
- Give the patient a way to contact you if they have questions
- Consider… “I’ve shared information that you were not expecting to hear today. You may come up with additional questions later on… if you do, feel free to write them down and we can discuss them at our next appointment.â€